At Neph Cure Inc., we are at the forefront of this precision shift in nephrology. We recognize that treating complex conditions like Membranous Nephropathy or IgA Nephropathy requires moving beyond general immunosuppression to target the exact mechanism driving the illness.
This professional post will illuminate the underlying membranous nephropathy causes, detail the crucial steps involved in IgAN diagnosis, and look ahead to the exciting developments in Apolipoprotein L1 treatment, demonstrating how targeted science is transforming the landscape of kidney care.
Part 1: The Immune Triggers—Membranous Nephropathy Causes
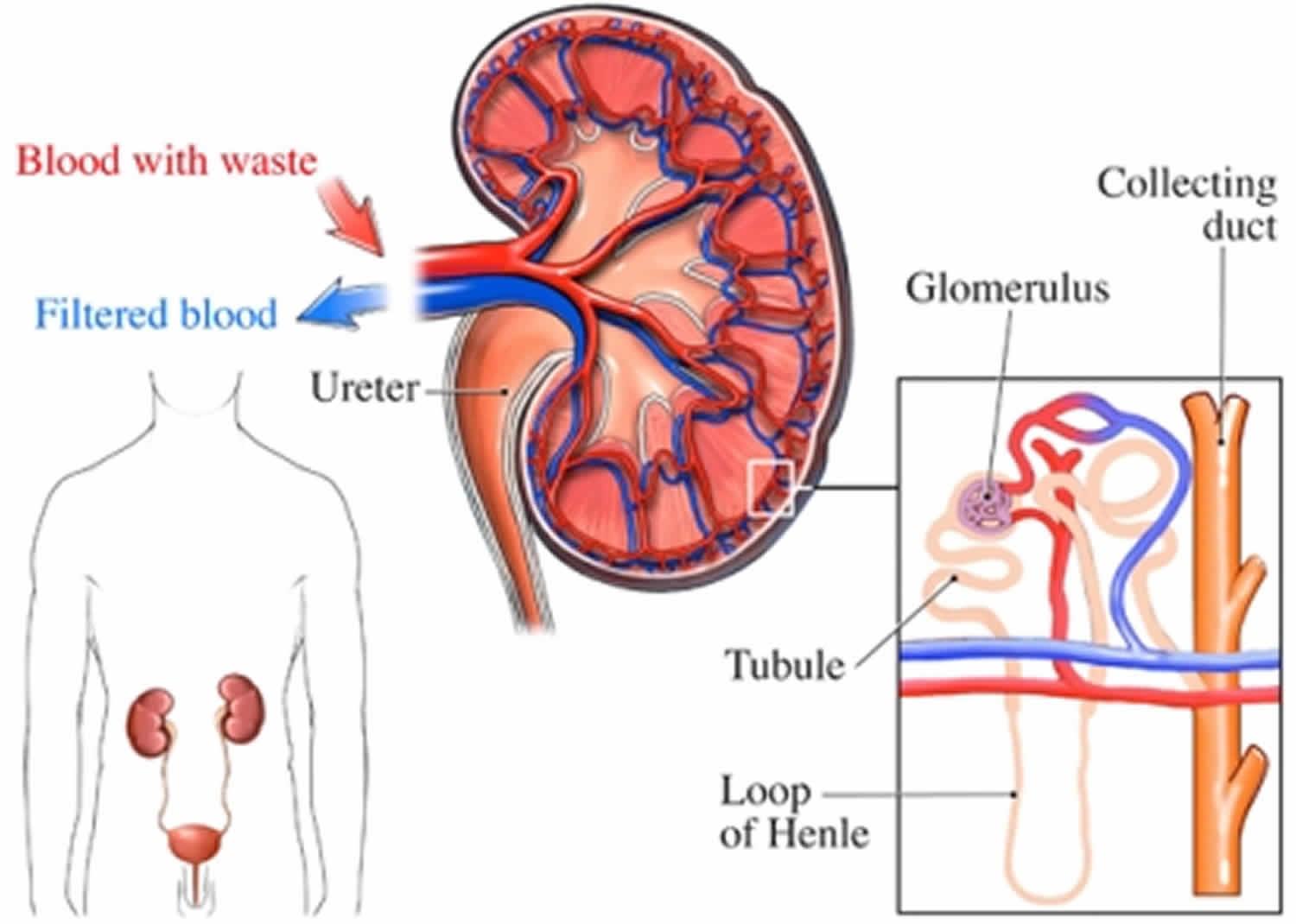
Membranous Nephropathy (MN) is a leading cause of nephrotic syndrome in adults, characterized by the formation of immune deposits on the outside of the glomerular basement membrane (the filter layer). Understanding the membranous nephropathy causes is the single most important step in choosing the right therapy.
Primary vs. Secondary Causes
The causes are broadly categorized based on whether the disease originates in the kidney's immune system or is a manifestation of a systemic issue:
-
Primary Membranous Nephropathy (pMN):
-
This is an autoimmune disease where the body mistakenly produces antibodies that attack specific proteins on the surface of the kidney's filtering cells (podocytes).
-
Anti-PLA2R Antibodies: In approximately 75% of pMN cases, the antibody targets the Phospholipase A2 Receptor (PLA2R), a protein found on the podocyte surface. The binding of this antibody triggers the immune deposit formation.
-
Non-PLA2R Antibodies: In the remaining cases, the antibodies may target other podocyte proteins, such as THSD7A (Thrombospondin Type-1 Domain-Containing 7A).
-
Key Insight: The ability to measure these circulating antibodies in the blood has revolutionized membranous nephropathy management, allowing doctors to diagnose the disease without a biopsy in many cases and track disease activity and response to treatment.
-
-
Secondary Membranous Nephropathy (sMN):
-
The immune deposits are triggered by an underlying systemic condition.
-
Common Causes:
-
Systemic Lupus Erythematosus (Lupus Nephritis): A systemic autoimmune disease.
-
Chronic Infections: Particularly Hepatitis B or syphilis.
-
Malignancy (Cancer): MN can sometimes be a paraneoplastic syndrome, signaling an underlying tumor.
-
Medications: Certain nonsteroidal anti-inflammatory drugs (NSAIDs) or gold salts (historically used for arthritis).
-
-
Treatment Focus: Treating secondary MN primarily involves treating the underlying condition (e.g., curing Hepatitis B or treating the cancer).
-
Part 2: Pinpointing the Problem—IgAN Diagnosis
IgA Nephropathy (IgAN) is the world's most common form of primary glomerulonephritis. It is caused by the deposition of abnormal IgA immune complexes in the kidney's mesangium (the structural core of the glomerulus). Because the early IgA nephropathy symptoms are often fleeting, achieving an accurate IgAN diagnosis is critical for preventing long-term kidney failure.
The Pathway to Diagnosis
While certain clinical features raise suspicion, a definitive IgAN diagnosis requires invasive testing:
-
Clinical Suspicion:
-
Gross Hematuria: The classic sign is visible blood in the urine occurring simultaneously with, or within 1-3 days after, an upper respiratory or gastrointestinal infection (a unique timing called "synpharyngitic hematuria").
-
Proteinuria: Persistent or increasing levels of protein in the urine.
-
Hypertension: Rising blood pressure.
-
-
Laboratory Markers:
-
Checking complement levels (usually normal in IgAN, unlike in C3G).
-
Measuring levels of galactose-deficient IgA1 (Gd-IgA1), the abnormal protein that drives the disease. This emerging blood test can provide strong supportive evidence of IgAN pathology.
-
-
The Gold Standard: Kidney Biopsy:
-
A definitive IgAN diagnosis requires a renal biopsy. Tissue samples are examined, and immunofluorescence testing must reveal the dominant deposition of IgA in the mesangium of the glomeruli.
-
The biopsy also allows for disease staging using the MEST-C scoring system, which assesses the level of inflammation and scarring and helps predict the patient's prognosis.
-
Achieving a prompt IgAN diagnosis is essential because effective treatment strategies—from blood pressure control to targeted immunosuppression—must be started early to prevent irreversible scarring.
Part 3: The Future is Genetic—Apolipoprotein L1 Treatment
Apolipoprotein L1 (APOL1) is a gene that carries high-risk variants (G1 and G2) that are strongly associated with aggressive forms of kidney disease, including FSGS and rapid kidney function decline, particularly in individuals of African descent. Until recently, there was no specific Apolipoprotein L1 treatment; management was limited to general blood pressure control (ACE inhibitors/ARBs).
Targeting the Toxic Gene Product
The research into Apolipoprotein L1 treatment represents one of the most exciting breakthroughs in precision nephrology. The goal is to neutralize the toxic effect of the high-risk APOL1 protein variants, which are thought to damage podocytes by forming toxic pores in the cell membrane.
-
APOL1 Inhibitors: Novel small-molecule drugs are currently in advanced clinical trials. These drugs are designed to directly inhibit the function of the APOL1 protein variant. By blocking the protein's ability to create pores and damage the podocyte, these inhibitors aim to stop the disease progression at its genetic and molecular source.
-
Significance:
-
This is the first true Apolipoprotein L1 treatment designed to intervene on the specific disease mechanism.
-
Success in these trials could dramatically reduce health disparities in kidney disease by providing a highly effective, targeted therapy for millions of at-risk individuals.
-
Genetic Testing is Key: Identifying which patients carry the two high-risk alleles (G1/G2) through genetic testing is the prerequisite step for enrolling patients in these trials and for future clinical application of this targeted therapy.
-
Neph Cure Inc.: Innovating for Precision in Kidney Health
The modern approach to kidney disease is moving away from generalized assumptions toward specific, molecular truths. Neph Cure Inc. is dedicated to helping patients and clinicians navigate this complex landscape.
By leveraging precision diagnostics—measuring PLA2R antibodies to identify the cause of Membranous Nephropathy, utilizing the biopsy to confirm IgAN diagnosis, and employing genetic testing to identify candidates for Apolipoprotein L1 treatment—we are helping to choose the most effective, least toxic path forward for every patient.
We are committed to the future where every kidney disease diagnosis is accompanied by a targeted treatment plan.
Ready to explore how molecular diagnostics are transforming the management of your kidney condition?
Contact Neph Cure Inc. today to learn about the latest advances in targeted treatments and diagnostic testing.