Urgent care centers handle a high volume of patients every day, providing fast medical treatment for non-emergency conditions. Due to walk-in visits, varied payer rules, multiple procedures in a single encounter, urgent care billing becomes a complex operational task. Accurate billing is essential for maintaining cash flow, reducing claim denials, supporting long-term financial stability. A structured approach involving urgent care billing services, strong documentation, reliable technology, plus efficient revenue management helps clinics achieve better reimbursement outcomes.
Understanding Urgent Care Billing
Urgent care billing refers to the process of converting patient encounters into compliant insurance claims. Each visit involves eligibility verification, service documentation, coding accuracy, timely claim submission. Billing challenges often arise due to incomplete documentation, incorrect coding levels, payer-specific policies.
Effective urgent care billing ensures services provided are translated into appropriate reimbursement while maintaining regulatory compliance.
Role of Urgent Care Billing Services
Urgent care billing services support clinics by managing administrative tasks related to claims, coding, payment follow-ups. These services reduce internal workload while improving billing accuracy.
Professional billing teams understand urgent care workflows, payer guidelines, documentation standards. Their expertise helps reduce rejected claims, speed up reimbursements, improve financial visibility.
Key Processes in Urgent Care Billing Services
Patient Eligibility Verification
Eligibility checks confirm active coverage before services begin. This step prevents avoidable denials caused by inactive plans or coverage exclusions.
Charge Capture Accuracy
Charge capture ensures all billable services are recorded properly. Missed charges result in revenue loss, especially in high-volume urgent care environments.
Coding Review
Coding review ensures documented services align with appropriate CPT codes. This process supports compliance while protecting revenue.
Claim Submission
Claims are submitted following payer-specific formats and timelines. Clean claim submission reduces processing delays.
Denial Management
Denial management focuses on identifying rejection causes, correcting issues, resubmitting claims promptly. Trend analysis helps prevent repeat denials.
Importance of Urgent Care CPT Coding
Urgent care CPT coding represents clinical services delivered during patient visits. Accurate coding reflects the complexity of care provided.
Evaluation and management codes, minor procedures, diagnostic services must align with documentation. Incorrect urgent care CPT coding increases audit risk or leads to underpayment. Precise coding ensures clinics receive appropriate reimbursement.
Common CPT Categories in Urgent Care
-
Evaluation and management visit levels
-
Minor surgical procedures
-
Wound care services
-
Injection administration
-
Diagnostic testing
Each category requires detailed documentation to support coding decisions.
How Urgent Care EHR Improves Billing Accuracy
Urgent care EHR systems store clinical documentation, patient demographics, insurance details in a centralized platform. Structured templates guide providers to capture required information consistently.
Accurate documentation within urgent care EHR supports proper coding, reduces missing data, improves claim acceptance rates. Automated prompts help minimize documentation gaps.
EHR Integration With Billing Workflows
Integrated urgent care EHR platforms allow seamless data flow from clinical notes to billing systems. This integration reduces manual entry, lowers error rates, accelerates claim generation.
Billing teams gain faster access to encounter details, supporting timely submission and follow-up.
Overview of Urgent Care Revenue Cycle Management
Urgent Care Revenue Cycle Management covers the entire financial process from patient registration to final payment posting. Strong revenue cycle control ensures predictable cash flow and operational efficiency.
Urgent Care RCM includes front-end verification, accurate coding, clean claim submission, payment reconciliation, denial resolution.
Stages of Urgent Care RCM
Front-End Operations
Front-end processes include patient registration, insurance verification, authorization checks. Errors at this stage affect downstream billing outcomes.
Coding and Charge Entry
Accurate coding reflects documented services. Charge entry must capture all billable items.
Claims Processing
Claims are tracked from submission through adjudication. Timely follow-up prevents aging accounts receivable.
Payment Posting
Payments must be posted correctly to maintain financial transparency.
Denial Resolution
Denial resolution identifies root causes, improves workflows, strengthens future billing performance.
Benefits of Efficient Urgent Care RCM
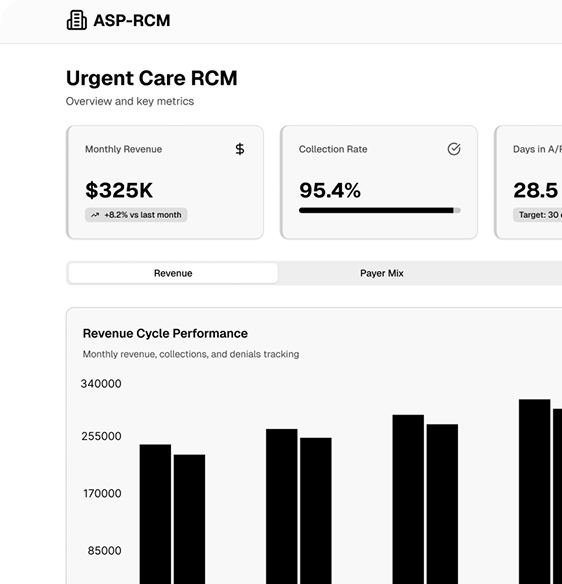
Efficient Urgent Care RCM improves reimbursement timelines, reduces revenue leakage, enhances operational control. Clinics gain insights into financial performance through reporting dashboards.
Better revenue management allows leadership to focus on patient care quality rather than administrative challenges.
Technology Role in Urgent Care Billing
Modern urgent care billing relies on automation, analytics, real-time reporting. Technology reduces manual work, improves accuracy, supports compliance.
Dashboards provide visibility into claim status, denial trends, revenue performance. This data-driven approach strengthens Urgent Care Revenue Cycle Management.
Compliance Challenges in Urgent Care Billing
Urgent care billing must comply with payer policies, coding guidelines, regulatory standards. Frequent updates increase complexity.
Professional billing teams stay current with changes, implement compliance checks, reduce audit risks. Compliance-focused workflows protect clinic revenue.
Why Clinics Outsource Urgent Care Billing Services
Many clinics choose urgent care billing services to manage complexity efficiently. Outsourcing provides access to experienced coders, advanced technology, scalable resources.
This approach improves accuracy while reducing staffing challenges and operational costs.
Future Outlook for Urgent Care Billing
Urgent care billing continues to evolve with healthcare technology advancements. Automation, predictive analytics, intelligent documentation tools enhance accuracy.
Urgent care EHR systems become more integrated with billing workflows, supporting real-time quality checks. Strong Urgent Care RCM remains critical for financial sustainability.
Conclusion
Urgent care billing requires structured workflows, accurate coding, reliable documentation to achieve consistent reimbursement. Urgent care billing services support clinics by managing complex processes with expertise. Urgent Care Revenue Cycle Management ensures smooth financial operations from patient intake through final payment. Accurate urgent care CPT coding combined with integrated urgent care EHR systems strengthens billing outcomes. With the right strategy, urgent care centers achieve financial stability, reduced denials, improved operational efficiency.