For decades, the standard approach to correcting amblyopia commonly known as lazy eye has been straightforward: cover the stronger eye with a patch to force the weaker one to work harder. While this method has helped countless children, it isn't always the perfect fit for everyone, especially as children grow older. As they enter their school years and beyond, the dynamics of their daily lives change, and so do their visual needs. Parents are increasingly looking for solutions that fit better with a modern, active lifestyle while still delivering results.
As we explore alternatives, it is important to understand how the landscape of lazy eye treatment is evolving. Newer insights into how the brain and eyes communicate have opened doors to methods that go beyond simple occlusion. For older children, these advancements offer hope for effective vision correction without the social and logistical hurdles often associated with wearing a patch.
The Shift in Understanding Amblyopia
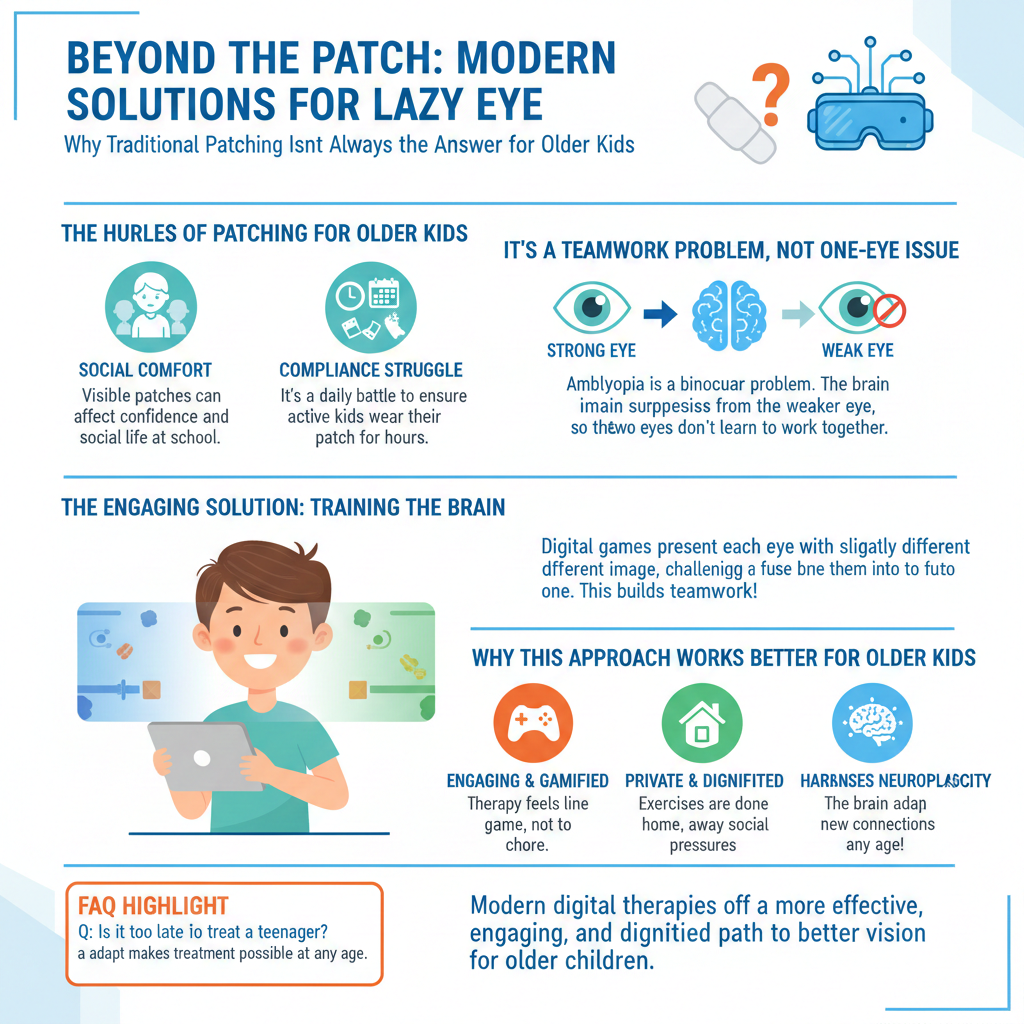
Traditionally, amblyopia was viewed primarily as a "monocular" problem an issue with just one eye. The logic followed that if you blocked the good eye, the "lazy" eye would be forced to strengthen. However, leading experts and vision scientists now understand that amblyopia is fundamentally a binocular problem. It is not just that one eye is weak; it is that the two eyes are not working together as a team. The brain actively suppresses the image from the weaker eye to avoid double vision or confusion.
When we simply patch the dominant eye, we are addressing the symptom (reduced acuity) but not necessarily the root cause (lack of binocular cooperation). This is why some children might see improvements while patching, only to have their vision regress once the patch is removed. They haven't learned to use both eyes simultaneously.
Challenges with Patching for Older Kids
While patching can be effective for toddlers, it presents a unique set of challenges for older children and teenagers. Understanding these hurdles is key to finding a more sustainable solution.
Social Comfort and Confidence
School-aged children are developing their social identities. Wearing an eye patch at school or during extracurricular activities can make a child feel self-conscious. At an age where blending in is often a priority, a visible medical device can sometimes lead to unwanted attention or feelings of isolation.
Preserving a child’s self-esteem is a crucial part of their overall well-being, and choosing a lazy eye treatment that feels “invisible” to their peers can make a significant difference in their comfort and happiness.
The Compliance Struggle
Let’s be honest: asking an energetic 10-year-old to wear a patch for several hours a day is a tall order. Older kids have homework, sports, and hobbies that require full visual awareness. Patching reduces their field of view and depth perception, making these activities frustrating or even difficult to perform. This often leads to "compliance battles" at home, where parents have to constantly remind or negotiate with their child to keep the patch on. A therapy that a child enjoys or at least doesn't dread is one they are more likely to stick with.
The Power of Binocular Therapy
This is where the exciting evolution of vision care comes into play. Modern approaches focus on "dichoptic" therapy. Instead of penalizing the strong eye, these methods encourage both eyes to work together.
Here is how it works: specialized digital platforms or games present different images to each eye independently. The dominant eye might see a lower-contrast image, while the weaker eye sees a higher-contrast image. The brain is then challenged to combine these two inputs into a single, clear picture.
Why This Appeals to Older Kids
-
It’s Engaging: Many of these therapies are gamified. Instead of sitting with a patch, a child might play a space adventure or a puzzle game on a tablet or computer.
-
It’s Active: The brain is actively learning to fuse images, which builds stronger neural pathways.
-
It’s Private: These exercises can often be done at home, meaning no one at school needs to know therapy is happening.
Neuroplasticity: The Brain’s Ability to Adapt
A common myth is that vision therapy is only effective during the "critical period" of early childhood, typically ending around age seven or eight. We now know this isn't the complete picture. The human brain possesses an incredible ability known as neuroplasticity—the capacity to reorganize itself by forming new neural connections throughout life.
While it is true that the brain is most malleable in early childhood, research has shown that teenagers and even adults can achieve significant visual improvements. By using engaging, high-stimulus activities that demand binocular integration, we can "wake up" the neural pathways associated with the weaker eye. This confirms that age is not a strict barrier to improvement. Older children have the advantage of better attention spans and a stronger understanding of the goals of therapy, which can actually enhance the effectiveness of these modern interventions.
Benefits of Digital and VR-Based Solutions
The integration of Virtual Reality (VR) and AI-driven software into vision care has been a game-changer. These tools offer a level of precision that an eye patch simply cannot match.
Personalized Difficulty Levels
Advanced software can adjust in real-time. As the child’s "lazy eye treatment" progress improves, the game creates new challenges, ensuring the brain is constantly being pushed just enough to adapt without causing frustration. This personalized approach ensures faster and more stable outcomes.
Better Depth Perception (Stereopsis)
Because digital therapies focus on using both eyes together, they often lead to better depth perception. This is the ability to judge distances accurately—a skill essential for catching a ball, driving a car, or navigating stairs safely. Patching alone often struggles to restore this 3D vision because it isolates the eyes rather than uniting them.
Positive Reinforcement
Digital programs often provide instant feedback. When a child successfully combines images, they earn points or advance levels. This positive reinforcement loop releases dopamine, which not only makes the therapy fun but also aids in the learning process of the brain.
Making the Right Choice for Your Child
Every child’s vision is unique, and what works for one might not work for another. However, for older children who have struggled with patching or for whom patching is socially difficult, exploring binocular, digital therapies is a wonderful step forward.
These modern solutions respect the child's emotional needs while employing cutting-edge science to retrain the brain. They move away from the "punishment" of the good eye and toward the "cooperation" of both eyes. If you are looking for a path that aligns with your child's lifestyle and takes advantage of the latest technology, looking beyond the patch might be the best decision for their visual future.
Conclusion
The journey to clear vision is no longer limited to a simple piece of fabric. As our understanding of the brain and vision has deepened, so too have our options for helping older children overcome amblyopia. By embracing methods that prioritize binocular cooperation and leverage the brain's natural plasticity, we can offer older kids a treatment experience that is effective, engaging, and dignity-preserving. It is a bright new era for vision therapy, one where technology and biology work hand-in-hand to help children see the world more clearly.
Frequently Asked Questions (FAQs)
Q: Is it too late to treat amblyopia in a teenager? A: No, it is not too late. While early treatment is often faster, the brain remains plastic throughout the teenage years and even into adulthood. Modern binocular therapies have shown great success in improving vision for older children and adults.
Q: How long does digital vision therapy take to show results? A: Results vary depending on the severity of the condition and compliance, but many users report noticing improvements in visual comfort and clarity within a few weeks of consistent practice. A typical program might last several months to ensure the changes are permanent.
Q: Can these new therapies replace glasses? A: Not necessarily. These therapies are designed to retrain the brain-eye connection. If a child has a refractive error like nearsightedness or farsightedness, they will likely still need glasses to ensure the image hitting the retina is focused. The therapy works in tandem with the glasses.
Q: Do these treatments require a doctor’s supervision? A: Yes. Even home-based digital therapies should be prescribed and monitored by an eye care professional. They will customize the program settings to your child's specific visual needs and track progress to ensure safety and effectiveness.
Q: Are video game-based therapies covered by insurance? A: Coverage varies significantly by provider and plan. It is best to check with your insurance company and your eye care specialist to understand the costs and potential reimbursement options available for vision therapy programs.